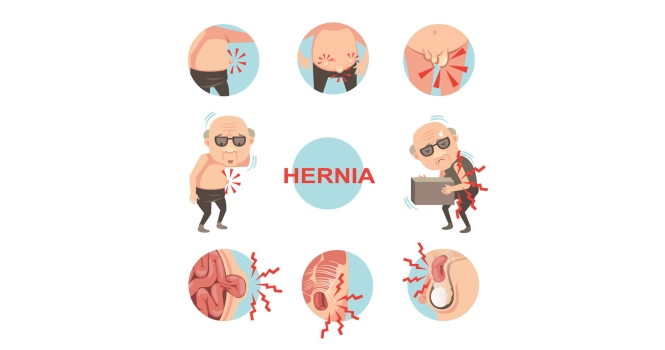
Hernias are a common medical condition affecting millions of people worldwide. Characterized by a protrusion of an organ or tissue through an abnormal opening, hernias can cause discomfort, pain, and even serious complications if left untreated. The definitive Treatment is Hernia Surgery.
The purpose of this article is to provide a comprehensive guide to understanding this prevalent condition and the surgical interventions available for its treatment.
What is Hernia?
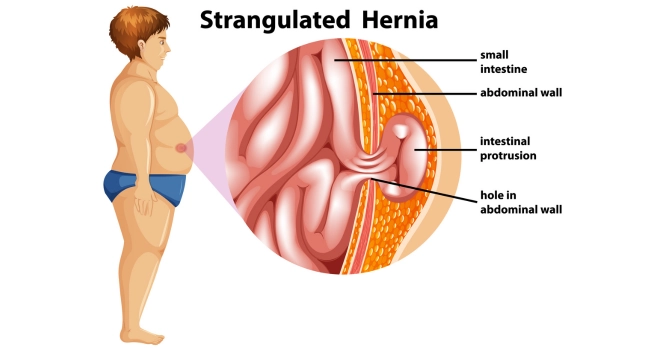
A hernia is a medical condition that occurs when an organ, intestine, or fatty tissue protrudes through a hole or a weak spot in the surrounding muscle or connective tissue. This often results in a visible lump or bulge, which may or may not be painful.
Hernias most commonly occur in the abdominal region but can also appear in the upper thigh, groin, and belly button areas. Depending on its location and severity, a hernia may require surgical intervention for repair and to prevent complications.
How the Human Body Structures are Involved in Hernia
The structures primarily involved are the muscles and connective tissues that make up the body’s walls, such as the abdominal wall. These walls serve as barriers that keep organs and tissues in their proper places.
When there is a weak spot or tear in these walls, it creates an opportunity for an organ or tissue to protrude through, forming a hernia. Depending on the type of hernia, different organs and tissues may be involved:
- Inguinal Hernia: Involves the intestines and the abdominal wall, specifically the inguinal canal in the groin area.
- Femoral Hernia: Involves the femoral canal, which is another groin area passage, and may contain intestine or fatty tissue.
- Umbilical Hernia: Involves the area around the belly button (umbilicus) and may contain intestine, fatty tissue, or fluid.
- Hiatal Hernia: Involves the diaphragm and the stomach. The stomach protrudes through the diaphragm into the chest cavity.
How a Hernia Develops
A hernia develops due to a combination of muscle weakness and strain. Here’s a simple explanation:
- Muscle Weakness: Over time, muscles can weaken due to factors like aging, congenital conditions, or previous surgeries. This creates vulnerable spots in the muscle or connective tissue walls.
- Straining: Activities that put pressure on the weak spots can trigger the development of a hernia. These activities can include lifting heavy objects, persistent coughing, or even straining during bowel movements.
- Protrusion: Due to the strain, the organ or tissue pushes through the weak spot, creating a bulge or lump, which is the hernia.
Statistical Data on Prevalence and Demographics
Hernias are a common medical condition, affecting millions worldwide. Here are some statistics to give you an idea of its prevalence and demographics:
- Inguinal Hernias: Account for about 75% of all hernias and are five times more common in men than in women.
- Hiatal Hernias: More common in people over 50 years of age. Approximately 10% of the population may have a hiatal hernia, although not all are symptomatic.
- Umbilical Hernias: Common in infants, affecting around 20% of newborns to some degree. They also occur in adults, particularly in those who are overweight or pregnant.
- Femoral Hernias: Relatively rare and occur more often in women, especially those who are pregnant or obese.
Understanding the prevalence and demographics can help in risk assessment and early diagnosis, leading to more effective treatment plans.
Types of Hernia
A. Inguinal Hernia
1. Definition and Description
An inguinal hernia occurs when a portion of the intestine or fatty tissue protrudes through a weak spot in the abdominal wall, specifically through the inguinal canal in the groin area. There are two types of inguinal hernias:
- Indirect Inguinal Hernia: This is the most common type and occurs when the intestine pushes through the internal inguinal ring, a weak spot that is present from birth.
- Direct Inguinal Hernia: This type occurs when the intestine pushes through a weakened area in the abdominal wall muscle, usually resulting from aging or an injury.
2. Causes and Risk Factors
The primary causes and risk factors for developing an inguinal hernia include:
- Muscle Weakness: Congenital weakness in the abdominal wall or weakening due to aging.
- Physical Strain: Activities that increase intra-abdominal pressure like lifting heavy objects, straining during bowel movements, or chronic coughing.
- Gender: Men are more susceptible due to the way the testicles descend, leaving a natural weak spot in the inguinal canal.
- Previous Hernia or Hernia Repair: Having had one hernia makes you more susceptible to developing another.
- Family History: A family history of hernias increases the risk.
- Chronic Constipation: Straining during bowel movements can contribute to the development of a hernia.
3. Prevalence and Demographics
Inguinal hernias are the most common type of hernia, accounting for about 75% of all abdominal hernias.
They are significantly more common in men, with a lifetime risk of 27% for men and 3% for women.
The risk increases with age, and they are also more common in individuals who are overweight or who engage in activities that involve heavy lifting or straining.
B. Femoral Hernia
1. Definition and Description
A femoral hernia occurs when a portion of tissue or an organ, such as a part of the intestine, protrudes through a weak spot in the abdominal wall into the femoral canal, which is located in the upper thigh near the groin.
Unlike inguinal hernias, femoral hernias are more likely to become strangulated, cutting off the blood supply to the herniated tissue, which is a medical emergency.
2. Causes and Risk Factors
The primary causes and risk factors for developing a femoral hernia include:
- Muscle Weakness: Aging or injury can weaken the abdominal wall and surrounding muscles, making them more susceptible to herniation.
- Physical Strain: Activities that increase intra-abdominal pressure, such as lifting heavy objects or chronic coughing, can contribute to the development of a femoral hernia.
- Gender: Femoral hernias are more common in women, particularly those who are pregnant or obese, due to the wider shape of the female pelvis.
- Previous Surgery: Surgical procedures near the femoral canal can weaken the area and make it more susceptible to hernias.
- Chronic Constipation: Straining during bowel movements can also be a contributing factor.
3. Prevalence and Demographics
Femoral hernias are relatively rare, accounting for only about 3% of all abdominal hernias.
They are more common in women, especially those who are pregnant or obese. The risk of developing a femoral hernia increases with age, and they are more commonly seen in adults rather than in children.
Femoral hernias are also more likely to occur on the right side of the body due to the position of the appendix, although they can occur on either side.
C. Umbilical Hernia
1. Definition and Description
An umbilical hernia occurs when a portion of the intestine or fatty tissue protrudes through a weak spot in the abdominal wall near the belly button (umbilicus).
This type of hernia is most commonly seen as a soft bulge at the navel and may vary in size.
In infants, the hernia may be noticeable only when the baby cries, coughs, or strains, causing the belly button to protrude.
2. Causes and Risk Factors
The primary causes and risk factors for developing an umbilical hernia include:
- Infancy: Many umbilical hernias develop due to an incomplete closure of the abdominal wall, noticeable shortly after birth.
- Adult Factors: In adults, factors like obesity, multiple pregnancies, and fluid in the abdominal cavity can contribute to the development of an umbilical hernia.
- Physical Strain: Activities that increase intra-abdominal pressure, such as lifting heavy objects or chronic coughing, can also be contributing factors.
- Previous Surgery: Surgical procedures near the umbilical area can weaken the abdominal wall, making it more susceptible to hernias.
3. Prevalence and Demographics
Umbilical hernias are common in infants, affecting around 10-20% of newborns to some degree. They are more common in African American infants and premature babies.
Most umbilical hernias in infants close on their own by the age of 1 to 2 years.
In adults, umbilical hernias are more common in women, particularly those who have had multiple pregnancies, and in individuals who are overweight. The condition can also occur in people with liver disease due to the accumulation of fluid in the abdominal cavity.
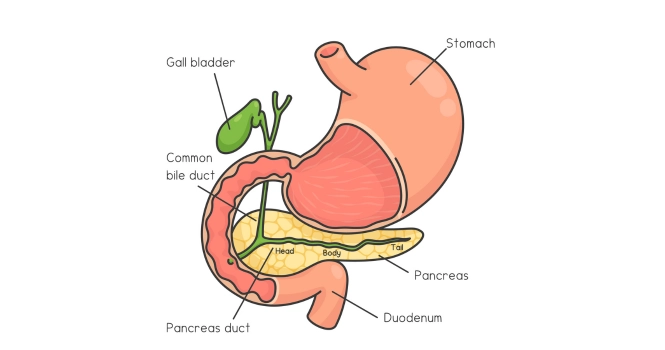
D. Hiatal Hernia
1. Definition and Description
A hiatal hernia occurs when the upper part of the stomach pushes through an opening in the diaphragm and into the chest cavity. The diaphragm is a large muscle that separates the abdomen from the chest and helps with breathing.
There are two main types of hiatal hernias:
- Sliding Hiatal Hernia: This is the most common type, where the stomach and the section of the esophagus that joins the stomach slide up into the chest.
- Paraesophageal Hiatal Hernia: Less common but more serious, this type occurs when part of the stomach squeezes through the hiatus and lies beside the esophagus, potentially leading to strangulation of the stomach.
2. Causes and Risk Factors
The primary causes and risk factors for developing a hiatal hernia include:
- Aging: The diaphragm’s muscle tissue can weaken with age, making older adults more susceptible.
- Increased Abdominal Pressure: Obesity, pregnancy, or excessive straining during bowel movements can increase intra-abdominal pressure.
- Injury or Surgery: Any trauma to the diaphragm or surgical procedures involving the upper abdomen can weaken the diaphragm.
- Congenital Factors: Some people are born with a larger hiatus, making them more susceptible to this type of hernia.
3. Prevalence and Demographics
Hiatal hernias are more common in people over the age of 50. It’s estimated that up to 60% of people by the age of 60 may have some form of hiatal hernia, although not all are symptomatic.
The condition is also more common in women and in individuals who are overweight or obese. However, the condition can occur at any age and in both genders.
E. Other Types of Hernia
1. Definition, Description, and Examples
Apart from the more common types of hernias like inguinal, femoral, umbilical, and hiatal, there are several other less common types:
- Incisional Hernia: Occurs through an incision or scar in the abdomen, often as a complication of abdominal surgery.
- Epigastric Hernia: Occurs between the navel and the lower part of the rib cage in the midline of the abdomen, usually involving fatty tissue rather than intestine.
- Spigelian Hernia: Occurs along the edge of the rectus abdominus muscle, several inches lateral to the middle of the abdomen.
- Obturator Hernia: A very rare hernia that occurs mostly in women, it protrudes through the obturator foramen in the pelvic bone.
2. Prevalence and Demographics
- Incisional Hernias: Occur in up to 20% of patients who have had abdominal surgery.
- Epigastric Hernias: Relatively rare, accounting for less than 1% of all hernias, and are more common in men.
- Spigelian Hernias: Extremely rare, making up about 1-2% of all abdominal hernias, and usually occur in those over the age of 40.
- Obturator Hernias: Extremely rare and are most commonly found in elderly women, often those with a history of multiple pregnancies.
Causes and Risk Factors of Hernia
A. Physical Strain and Heavy Lifting
Physical strain and heavy lifting are among the most common causes and risk factors for developing various types of hernias, particularly inguinal and incisional hernias. Here’s how they contribute to the condition:
Mechanism:
When you lift a heavy object, the action increases intra-abdominal pressure. This pressure pushes against weak spots in the abdominal wall or other susceptible areas.
If the muscle or tissue is already weakened due to other factors like aging, previous surgery, or congenital defects, it may not be able to withstand this pressure. As a result, an organ or tissue may protrude through the weak spot, forming a hernia.
Risk Amplification:
- Incorrect Lifting Technique: Lifting heavy objects without proper form can significantly increase the risk of developing a hernia. Using your back instead of your legs to lift, for example, can put undue strain on your abdominal area.
- Occupational Hazards: Jobs that require frequent heavy lifting, pushing, or pulling can increase the risk of hernias over time due to repeated stress on relevant muscle groups.
- Sports: Athletes or individuals who engage in high-intensity sports that involve lifting weights or sudden, forceful movements may also be at higher risk.
Pre-existing Conditions:
People with pre-existing conditions that weaken the abdominal wall or increase intra-abdominal pressure, such as obesity or chronic obstructive pulmonary disease (COPD), are at higher risk when engaging in activities involving physical strain or heavy lifting.
Prevention:
- Proper Lifting Techniques: Always bend at the knees, not the waist, when lifting heavy objects. Keep the object close to your body and lift using your leg muscles.
- Core Strengthening: Exercises that strengthen the abdominal and back muscles can help support the area and may reduce the risk of developing a hernia.
- Consult a Physician: If you have a history of hernias or other risk factors, consult a healthcare provider for personalized advice before engaging in heavy lifting or strenuous physical activity.
B. Chronic Coughing and Sneezing
Chronic coughing and sneezing are less commonly recognized but significant factors that can contribute to the development of a hernia. Here’s how they play a role:
Mechanism:
Much like heavy lifting, chronic coughing and sneezing can increase intra-abdominal pressure.
Each cough or sneeze forces the abdominal muscles to contract sharply, pushing against the internal organs and any weak spots in the abdominal wall or diaphragm. Over time, this repeated pressure can cause a hernia to form or exacerbate an existing one.
Risk Amplification:
- Underlying Medical Conditions: Chronic respiratory conditions like asthma, COPD, or chronic bronchitis often involve persistent coughing, thereby increasing the risk of developing a hernia.
- Allergies: Seasonal or chronic allergies that cause frequent sneezing can also contribute to hernia formation.
- Smoking: Smoking is often associated with chronic coughing and can be a contributing factor.
Pre-existing Conditions:
Individuals with pre-existing weak spots in their abdominal wall or diaphragm are at higher risk. This includes those with previous hernias, abdominal surgeries, or congenital muscle weaknesses.
Prevention:
- Manage Underlying Conditions: Effective management of respiratory conditions or allergies can reduce coughing and sneezing, thereby lowering the risk.
- Avoid Irritants: Avoiding smoke and other respiratory irritants can help manage chronic coughing.
- Consult a Physician: If you have chronic coughing or sneezing, it’s advisable to consult a healthcare provider for diagnosis and management, especially if you have other hernia risk factors.
C. Obesity
Obesity is a significant risk factor for the development of various types of hernias, including inguinal, umbilical, and incisional hernias. Here’s how obesity contributes to the condition:
Mechanism:
Obesity increases intra-abdominal pressure due to the excess weight carried in the abdominal area. This constant pressure pushes against weak spots in the abdominal wall or other susceptible areas, such as the diaphragm in the case of hiatal hernias.
The increased pressure can lead to the protrusion of an organ or tissue through these weak spots, resulting in a hernia.
Risk Amplification:
- Multiple Hernias: Obesity increases the risk of not just one but potentially multiple hernias due to the widespread increase in intra-abdominal pressure.
- Complications: Obesity can also make hernia repair more complicated, increasing the risk of postoperative complications such as wound infections or hernia recurrence.
- Associated Conditions: Obesity often coexists with other conditions like diabetes or respiratory issues that can independently increase hernia risk.
Pre-existing Conditions:
Individuals who are obese and also have other risk factors, such as a history of abdominal surgery, chronic cough, or family history of hernias, are at even higher risk of developing a hernia.
Prevention:
- Weight Management: Losing weight through a balanced diet and regular exercise can significantly reduce the risk of developing a hernia and can improve outcomes if surgery is needed.
- Core Strengthening: Exercises that strengthen the abdominal wall can provide additional support, potentially reducing the risk of hernia development.
- Consult a Physician: If you are obese and concerned about the risk of developing a hernia, consult a healthcare provider for a comprehensive risk assessment and personalized advice on weight management and other preventive measures.
D. Aging
Mechanism:
As people age, muscle tissue naturally weakens and loses elasticity. This weakening can make the abdominal wall or other areas more susceptible to hernias, especially when combined with increased intra-abdominal pressure.
Risk Amplification:
- Multiple Health Issues: Older adults often have multiple health conditions that can contribute to hernia risk, such as chronic cough or constipation.
- Previous Hernias: The risk of hernia recurrence increases with age.
Prevention:
- Regular Check-ups: Older adults should have regular medical check-ups to monitor for hernias, especially if they have other risk factors.
- Physical Activity: Engaging in regular, moderate exercise can help strengthen the abdominal wall and may reduce the risk of hernias.
E. Previous Surgical Wound
Mechanism:
Surgical incisions can weaken the abdominal wall, making it more susceptible to hernias, commonly known as incisional hernias.
Risk Amplification:
- Type of Surgery: Some surgeries, like abdominal or pelvic surgeries, pose a higher risk for hernia development.
- Postoperative Complications: Infections or other complications can further weaken the surgical site.
Prevention:
- Follow Postoperative Guidelines: Adhering to postoperative care guidelines can minimize strain on the surgical site and reduce the risk of a hernia.
F. Pregnancy:
Mechanism
Pregnancy increases intra-abdominal pressure and can stretch and weaken abdominal muscles, increasing the risk of hernias such as umbilical or femoral hernias.
Risk Amplification:
- Multiple Pregnancies: The risk increases with each subsequent pregnancy.
- Pre-existing Hernias: Pregnancy can exacerbate any pre-existing hernias.
Prevention:
- Prenatal Care: Regular prenatal check-ups can help monitor for hernias.
- Postpartum Exercise: Consult a healthcare provider about safe ways to strengthen the abdominal wall after giving birth.
G. Genetic Factors
Mechanism:
Some people are born with weaker abdominal walls or other predispositions that make them more susceptible to hernias.
Risk Amplification:
- Family History: A family history of hernias significantly increases the risk.
Prevention:
- Early Screening: If hernias are common in your family, early screening and regular check-ups are advisable.
H. Lifestyle Factors (e.g., Smoking)
Mechanism:
Smoking can lead to chronic coughing, which increases intra-abdominal pressure. It also impairs wound healing, making postoperative hernias more likely.
Risk Amplification:
- Chronic Respiratory Issues: Smoking can lead to conditions like COPD, which involve chronic coughing.
- Poor Wound Healing: Smoking impairs blood flow, making surgical wounds heal more slowly and increasing the risk of hernia post-surgery.
Prevention:
- Quit Smoking: Quitting smoking can reduce cough and improve overall tissue health, reducing the risk of hernias.
Symptoms of Hernia
A. Early Symptoms and Warning Signs
Early symptoms of a hernia can be subtle and may include:
- A small, localized bulge in the abdominal or groin area
- Mild discomfort or a feeling of heaviness in the affected area
- A dull ache that worsens with strain, lifting, or prolonged standing
B. Symptoms Related to Different Types of Hernia
- Inguinal Hernia: Often presents as a lump in the groin area, which may disappear when lying down and become more apparent when standing or straining.
- Femoral Hernia: Similar to inguinal hernias but located slightly lower; may cause groin or thigh pain.
- Umbilical Hernia: Usually manifests as a bulge around the belly button, often noticeable when the baby cries or an adult strains.
- Hiatal Hernia: Symptoms may include heartburn, difficulty swallowing, and chest pain.
- Incisional Hernia: A bulge near or at the site of a previous surgical incision, often accompanied by discomfort or pain.
C. Complications and Emergency Symptoms
- Strangulation: Severe, sudden pain with a firm, immovable lump indicates that the hernia may be strangulated, cutting off blood supply to the affected tissue.
- Obstruction: Nausea, vomiting, and severe abdominal pain may indicate bowel obstruction.
- Skin Redness or Discoloration: This could indicate an infection or compromised blood supply and requires immediate attention.
D. When to Seek Medical Attention
- Persistent or Worsening Symptoms: Any lump, discomfort, or other symptoms that persist or worsen should be evaluated by a healthcare provider.
- Pain: While some hernias are painless, the onset of pain usually necessitates prompt medical evaluation.
- Emergency Symptoms: Strangulation and obstruction are medical emergencies requiring immediate attention.
Diagnosis of Hernia
A. Physical Examination
The first step in diagnosing a hernia usually involves a physical examination by a healthcare provider. During this exam:
- The provider may ask you to stand and cough or strain, which can make a hernia more prominent.
- The area around the suspected hernia will be palpated to assess the size, location, and severity.
- In the case of inguinal hernias, a physical exam may include checking for a bulge in the groin area.
B. Imaging Tests (Ultrasound, CT Scan, etc.)
Imaging tests can provide a more detailed view of the hernia and surrounding structures:
- Ultrasound: Often used for initial evaluation, especially for softer, less obvious hernias.
- CT Scan: Provides detailed cross-sectional images and is particularly useful for complex or recurrent hernias.
- MRI: May be used in more complicated cases where high-resolution images are needed for surgical planning.
C. Endoscopy
Endoscopy is primarily used for diagnosing hiatal hernias:
- A flexible tube with a camera is inserted down the esophagus to examine the stomach and esophageal junction.
- This allows the healthcare provider to assess the size of the hernia and any associated complications like inflammation or ulceration.
D. Role of Patient’s History in Diagnosis
A thorough patient history can provide valuable clues for diagnosing a hernia:
- Previous Surgeries: A history of abdominal surgeries can indicate a higher risk for incisional hernias.
- Symptoms: The onset, duration, and nature of symptoms can help differentiate between types of hernias and associated complications.
- Family History: A family history of hernias can be a significant factor in diagnosis and risk assessment.
- Lifestyle Factors: Information about occupation, physical activities, and other lifestyle factors can help in understanding the potential causes and risks.
Treatment Options for Hernia
A. Watchful Waiting (for Asymptomatic Hernias)
For small, asymptomatic hernias that are not causing discomfort or complications, a “watchful waiting” approach may be advised:
- Regular Monitoring: Periodic check-ups are essential to monitor the size and symptoms of the hernia.
- Symptom Tracking: Patients are usually advised to keep track of any changes in symptoms and report them to their healthcare provider.
B. Lifestyle Changes and Self-Care Measures
Lifestyle modifications can help manage symptoms and may slow the progression of a hernia:
- Weight Loss: Reducing body weight can decrease intra-abdominal pressure, reducing hernia symptoms and the risk of complications.
- Dietary Changes: For hiatal hernias, avoiding spicy foods, caffeine, and alcohol can reduce symptoms like heartburn.
- Proper Lifting Techniques: Using proper form when lifting heavy objects can reduce strain on hernia-prone areas.
- Core Strengthening: Exercises that strengthen the abdominal muscles can provide better support to the area.
C. Medications
While medications can’t repair a hernia, they can sometimes help manage symptoms:
- Pain Relief: Over-the-counter pain medications like acetaminophen or ibuprofen may be used for mild discomfort.
- Antacids and Acid Reducers: For hiatal hernias, medications like antacids, H2 blockers, or proton pump inhibitors can help manage symptoms like heartburn and acid reflux.
- Stool Softeners: For hernias exacerbated by straining during bowel movements, stool softeners can help.
D. Surgical Procedures
Surgery is often the only definitive treatment for repairing a hernia. The choice of surgical technique depends on various factors, including the type, size, and location of the hernia, as well as the patient’s overall health.
1. Open Surgery
- Procedure: In open hernia repair, a single large incision is made in the abdomen or groin. The protruding tissue is pushed back into place, and the weakened area is stitched and often reinforced with a synthetic mesh.
- Recovery: Recovery time is generally longer compared to other surgical methods, and there may be more postoperative pain.
- Suitability: Open surgery is often used for larger or more complicated hernias, or for patients who have had previous abdominal surgeries.
2. Laparoscopic Surgery
- Procedure: Several small incisions are made to allow for the insertion of surgical instruments and a laparoscope, a small camera that guides the surgeon. The hernia is repaired in a manner similar to open surgery but through these smaller incisions.
- Recovery: Typically has a shorter recovery time and less postoperative pain compared to open surgery.
- Suitability: Best for smaller hernias and is often not recommended for complex or recurrent hernias.
3. Robotic-assisted Surgery
- Procedure: Similar to laparoscopic surgery but performed using a robotic system that the surgeon controls. This allows for greater precision and control during the procedure.
- Recovery: Recovery time is comparable to laparoscopic surgery but may vary depending on the complexity of the hernia and the patient’s overall health.
- Suitability: Useful for complex hernias where greater precision is needed, or in areas that are difficult to reach with traditional laparoscopic instruments.
Each surgical approach has its own risks and benefits, and the choice of method will depend on individual patient factors.
It’s crucial to discuss all available options with your healthcare provider to determine the most appropriate treatment for your hernia.
E. Comparison of Surgical Techniques
- Open Surgery:
- Pros: Suitable for larger, more complex hernias; can be performed even if the patient has had previous abdominal surgeries.
- Cons: Longer recovery time; higher risk of postoperative pain and complications like wound infection.
- Laparoscopic Surgery:
- Pros: Shorter recovery time; less postoperative pain; smaller scars.
- Cons: Not suitable for all types of hernias; may have a higher recurrence rate for certain hernias.
- Robotic-assisted Surgery:
- Pros: High precision; better visualization for the surgeon; potentially shorter hospital stay.
- Cons: Expensive; not widely available; learning curve for surgeons.
F. Risks and Complications of Treatment
- Infection: Risk of wound infection post-surgery.
- Recurrence: The hernia may recur, requiring additional surgeries.
- Nerve Damage: Potential for nerve damage leading to chronic pain.
- Adverse Reactions: Risks associated with anesthesia or other medications used during surgery.
- Strangulation: Delay in treatment can lead to strangulation of the herniated tissue, a medical emergency.
G. Post-surgery Care and Recovery
- Pain Management: Pain is common after hernia surgery and is usually managed with medications as prescribed by the healthcare provider.
- Activity Restrictions: Patients are generally advised to avoid strenuous activities and heavy lifting for a certain period post-surgery.
- Wound Care: Keeping the surgical site clean and dry is crucial for preventing infection.
- Follow-up Visits: Regular check-ups are essential for monitoring the healing process and for early detection of any complications or recurrence.
- Diet and Lifestyle: Resuming a balanced diet and gradual physical activity as advised by the healthcare provider can aid in faster recovery and may help prevent recurrence.
Understanding the different surgical techniques, their risks and complications, and what to expect post-surgery can help you make an informed decision about your hernia treatment.
Preventive Measures
A. Lifestyle Modifications
B. Proper Lifting Techniques
C. Importance of Regular Physical Activity
D. Balanced Diet
E. Regular Check-ups
Prevention is often the best approach to managing the risk of developing a hernia. Here are some preventive measures that can be effective:
A. Lifestyle Modifications
- Weight Management: Maintaining a healthy weight can reduce intra-abdominal pressure, one of the key factors in hernia development.
- Smoking Cessation: Quitting smoking can reduce chronic coughing, another risk factor for hernias.
- Avoid Straining: Whether during bowel movements or other activities, avoid excessive straining to reduce abdominal pressure.
B. Proper Lifting Techniques
- Use Your Legs: Always bend at the knees, not the waist, when lifting heavy objects.
- Keep it Close: Hold the object close to your body as you lift.
- Don’t Twist: Avoid twisting your body while lifting, as this can put extra strain on your abdominal muscles.
C. Importance of Regular Physical Activity
- Core Strengthening: Exercises that focus on strengthening the abdominal and back muscles can provide better support to the abdominal wall.
- Cardiovascular Exercise: Regular aerobic exercise can help in maintaining a healthy weight, thereby reducing hernia risk.
D. Balanced Diet
- High-Fiber Foods: A diet rich in fiber can prevent constipation and reduce straining during bowel movements, which can help prevent certain types of hernias.
- Avoid Overeating: Overeating can lead to weight gain and increase the risk of hiatal hernias due to increased pressure on the diaphragm.
E. Regular Check-ups
- Early Detection: Regular medical check-ups can help in the early detection of hernias, making them easier to treat.
- Risk Assessment: If you have risk factors like a family history of hernias, previous abdominal surgeries, or other medical conditions that increase your risk, regular check-ups are even more crucial.
By adopting these preventive measures, you can significantly reduce your risk of developing a hernia or experiencing complications from an existing one.
Always consult your Doctor for personalized advice according to your medical condition.