Cosmetic surgeries have become increasingly common, with procedures ranging from breast enlargement to facial enhancements and intimate reconstructions.
Hymenoplasty Surgery, commonly known as hymen repair surgery, is a procedure that has garnered attention and debate in various cultural and medical circles.
Whether driven by personal, cultural, or medical reasons, understanding hymenoplasty is crucial for those considering it or simply seeking to be informed.
Note: It’s crucial to consult a qualified medical professional if you’re considering hymenoplasty. The procedure involves surgical intervention and carries both medical and psychological risks.
Turning to unqualified individuals or “quacks” for such a delicate operation can result in severe complications, including infection, excessive bleeding, and even chronic pain. An unhygienic environment further elevates these risks. Always ensure that you’re dealing with an accredited and experienced surgeon in a reputable clinic or hospital.
This not only ensures that you receive the highest standard of care but also that you are making an informed decision about your body and health.
What is Hymen?
The hymen is a thin piece of mucosal tissue that surrounds or partially covers the external vaginal opening. It forms part of the vulva, or external genitalia, and is similar in structure to the vagina.
The hymen varies in size, shape, and form from person to person.
The presence, condition, or shape of the hymen has been historically, and inaccurately, used to determine if a woman or girl has had vaginal intercourse.
This belief is rooted in cultural and religious traditions rather than scientific facts. There are several reasons why:
- Natural variations: Some girls are born without a noticeable hymen.
- Stretching: The hymen can be stretched open with activities like riding a bike, horseback riding, inserting a tampon, or undergoing a medical examination.
- Tears and injuries: Physical injuries might cause tears in the hymen.
- Normal wear and tear: Over time, the hymen may erode due to normal hormonal changes and vaginal discharges.
It’s important to note that the state of the hymen is not a reliable indicator of virginity or past sexual activities. Relying on such notions can perpetuate harmful myths and stigmas about women and their bodies.
What is the use of Hymen?
The exact purpose of the hymen is not entirely clear and has been a subject of debate. However, here are a few theories and considerations regarding its role:
1. Evolutionary Vestige: Some scientists believe the hymen might be a vestigial structure, meaning it may have had a function in our evolutionary past but doesn’t have a specific function now.
2. Protection: One theory suggests that the hymen might help protect the infant’s vagina from contaminants, thus reducing the risk of infections. Given that the hymen is more prominent in infants and tends to change or diminish over time, this theory might have some basis.
3. No Specific Function: Just as with other body parts like the appendix, it’s possible the hymen doesn’t have a significant function. Not every physical trait or feature needs to have a specific purpose.
4. Cultural and Societal Significance: Over the course of history, in various cultures, the hymen has taken on significant cultural, social, and even religious meanings, particularly as a symbol of virginity. However, these beliefs are not rooted in scientific understanding and can be harmful.
It’s crucial to reiterate that the presence or state of the hymen is not a reliable indicator of virginity or past sexual activity. While it might have some evolutionary or protective function, its precise role remains unclear.
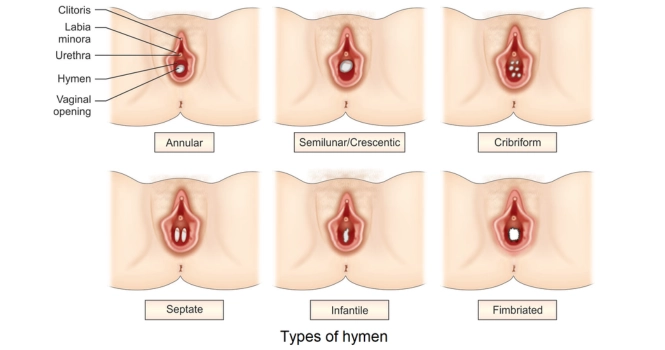
Types of Hymen
The hymen can have various shapes and sizes, and there are different types of hymens based on their morphology. Here are some common types:
1. Annular (Circular) Hymen: This is the most common type. The hymen forms a ring around the vaginal opening.
2. Crescentic Hymen: The hymenal tissue forms a crescent shape, usually at the bottom or top of the vaginal opening.
3. Fimbriated Hymen: The hymen has irregular, finger-like projections.
4. Septate Hymen: There are one or more bands of tissue stretching across the vaginal opening, creating a bridge or septum. This can sometimes pose issues for menstrual flow or tampon insertion and might need surgical intervention.
5. Microperforate Hymen: The vaginal opening is almost completely covered by the hymen, with only a small hole to allow menstrual blood to flow out. This type can also sometimes require medical intervention.
6. Imperforate Hymen: The vaginal opening is entirely covered by the hymen. An imperforate hymen can pose significant issues, especially during the onset of menstruation, as the menstrual blood cannot flow out, leading to a buildup in the vagina (hematocolpos). This condition usually needs surgical correction.
7. Denticulate Hymen: The hymen has a saw-toothed appearance with multiple notches.
8. Parous Introitus: Refers to a hymenal configuration typically seen after vaginal childbirth. The hymen is often stretched or torn and might have fleshy tags or remnants.
It’s important to note that the presence, shape, or size of the hymen can vary widely among individuals and does not indicate anything about one’s sexual history or activity.
Some of these configurations, like the imperforate or septate hymen, might need medical intervention due to the associated health issues, while others are simply natural variations without any implications for health or function.
What is Hymenoplasty Surgery?
Hymenoplasty, sometimes referred to as “hymen repair” or “revirgination” surgery, is a surgical procedure that aims to repair or reconstruct the hymen.
The primary motivation for the surgery is often cultural or religious, rooted in the belief in some societies that an intact hymen is a symbol of virginity and purity.
The procedure typically involves:
1. Stitching Together Remnants: If remnants of the hymen are still present, they can be stitched together to narrow the vaginal opening. After this procedure, any subsequent vaginal penetration might result in bleeding.
2. Creating a New Hymen: If there are insufficient hymenal remnants, a new hymen can be created using tissues from the vaginal lining or using a synthetic/biological insert.
The procedure is typically done under local or general anesthesia and usually takes a short amount of time, with patients often able to return home on the same day. Recovery time can vary, but most patients are advised to avoid strenuous activities for a few weeks.
It’s important to note several things about Hymenoplasty Surgery:
Temporary Nature: The constructed or repaired hymen can be torn or broken by various activities, not just intercourse, making the procedure temporary in nature.
Hymenoplasty Procedure Details
Pre-surgery consultations and preparations:
- Medical Consultation: The first step is to consult with a qualified gynecologist or plastic surgeon who specializes in hymenoplasty. During this consultation, the surgeon will discuss the patient’s reasons for seeking the procedure and evaluate the feasibility of the surgery.
- Physical Examination: The surgeon will conduct a physical examination of the genital area to assess the remnants of the hymen and decide on the best surgical technique.
- Medical History: It’s essential to discuss any allergies, previous surgeries, current medications, and overall health to minimize the risk of complications.
- Informed Consent: The patient should be informed of the risks, benefits, and expected outcomes of the surgery. It’s crucial to have a clear understanding of what the procedure can and cannot achieve.
- Pre-operative Instructions: These may include refraining from taking certain medications, avoiding smoking, and following specific hygiene practices before the surgery.
Surgical techniques and methods:
- Simple Repair: If there are enough hymenal remnants, they can be stitched together. This procedure is relatively straightforward and involves suturing the torn edges.
- Hymen Reconstruction: In cases where the remnants are insufficient, tissue from the vaginal lining (vaginal mucosa) can be used to create a new hymen. Alternatively, synthetic or biological materials may be used to reconstruct the hymenal membrane.
- Alloplant Insertion: If both the above methods aren’t feasible, a biomaterial may be inserted into the vagina, which acts as a pseudo-hymen. Some versions of this method also incorporate blood capsules to mimic bleeding during subsequent intercourse.
- Anesthesia: The procedure is typically performed under local anesthesia, but general anesthesia can be used if the patient or surgeon prefers.
Post-surgery care and recovery:
- Immediate Recovery: After the procedure, the patient might experience some pain, swelling, and minor bleeding. Over-the-counter pain relievers or prescribed medications can help manage pain.
- Activity Limitations: It’s advised to avoid strenuous physical activity, especially activities that put pressure on the genital area, for at least a few weeks. Sexual intercourse should be avoided for about 6-8 weeks or as recommended by the surgeon.
- Hygiene: Maintaining cleanliness in the operated area is essential to prevent infections. The surgeon will provide specific instructions regarding cleaning and bathing.
- Follow-up Visits: These are necessary to ensure that the area is healing correctly and to address any complications or concerns.
- Potential Complications: As with any surgery, there are risks of complications, such as infections, adverse reactions to anesthesia, excessive bleeding, or unsatisfactory results. It’s essential to be aware of these risks and address any issues promptly.
It’s crucial to follow the surgeon’s post-operative care instructions carefully to ensure proper healing and avoid complications.
Risks and Considerations of Hymenoplasty
Potential complications and risks:
Like any surgery, hymenoplasty comes with potential complications and risks. These include infection at the surgical site, excessive or prolonged bleeding, and scarring that may require further treatment.
Additionally, there’s the possibility of an adverse reaction to anesthesia, unsatisfactory results in the hymen’s appearance or function, and, in rare instances, chronic pain in the operated area.
Ethical considerations:
Hymenoplasty also raises ethical and social concerns. The procedure can perpetuate myths about virginity and an intact hymen, further stigmatizing women.
Additionally, societal or familial pressures may coerce some women into undergoing the surgery, rather than it being a personal choice.
This blurs the line between medical necessity and cultural practice, sparking ethical debates about the appropriateness of performing such procedures for non-medical reasons.
Factors to consider when choosing a surgeon or clinic:
When choosing a surgeon or clinic for hymenoplasty, consider the following key factors: Verify the surgeon’s qualifications and experience.
Research the reputation of the clinic and surgeon through reviews and testimonials. Ensure the facility is accredited by relevant medical boards.
Prioritize a thorough consultation process for informed consent. Check the post-operative care offered and ensure cost transparency to avoid hidden fees.
When considering hymenoplasty, it’s essential to weigh the benefits against potential risks and ethical implications. Anyone thinking about the procedure should be adequately informed, making a decision based on personal values and beliefs rather than external pressures.
Frequently Asked Questions
Hymenoplasty is typically performed under local or general anesthesia, which means the patient should not feel pain during the procedure. However, post-operatively, some discomfort, swelling, and mild pain might be experienced, which can be managed with prescribed painkillers.
Hymenoplasty surgery aims to repair or reconstruct the hymen, a thin membrane at the entrance of the vagina. The primary motivations for this surgery are often cultural or religious, where an intact hymen is considered a symbol of virginity and purity. It might also be sought for personal or psychological reasons, such as after trauma.
The results of a hymenoplasty, in terms of the physical presence of a hymen, can last until the membrane is disrupted or torn. This can happen during sexual intercourse, but also through non-sexual activities like vigorous exercise or tampon insertion. If the primary goal is to have the hymen intact for a specific event, such as a wedding night, it’s advisable to schedule the surgery reasonably close to that time.
Yes, a woman can bleed after hymenoplasty, especially if the surgery was designed to simulate the natural hymen’s properties. Some techniques involve the insertion of a blood capsule to ensure bleeding upon subsequent intercourse. However, it’s essential to note that not all women bleed after the rupture of their original hymen, and the same applies post-hymenoplasty.
Yes, you can walk after a hymenoplasty, but it’s advisable to limit physical activity and avoid strenuous exercises for a few days to prevent discomfort and ensure proper healing.
The risks associated with hymenoplasty include infection, excessive bleeding, scarring, adverse reactions to anesthesia, unsatisfactory results, and chronic pain or discomfort in the operated area. As with any surgical procedure, it’s essential to choose a qualified surgeon to minimize these risks.
Hymenoplasty is typically sought by women for cultural, religious, personal, or psychological reasons. Some women undergo the procedure to conform to societal expectations regarding virginity and purity, while others might choose the surgery for personal reasons, such as emotional healing after trauma.
Hymenoplasty recreates the hymen, but like the natural hymen, it can rupture or tear upon penetration or due to other activities. So, while the surgery’s effects can last until the reconstructed hymen is disrupted, it is not permanent.
After hymen surgery, the patient may experience mild pain, swelling, and minor bleeding. It’s essential to maintain cleanliness in the operated area to prevent infections. Sexual intercourse and tampon usage should be avoided for about 6-8 weeks or as recommended by the surgeon. There will also be follow-up visits to ensure proper healing and address any complications or concerns.